What Causes Lower Back Pain in Females?
What Causes Lower Back Pain in Females - Unraveling the Mystery!
Lower back pain in women is common, but it is not trivial. Many women experience lower back pain that ranges from dull soreness to sharp, stabbing sensations on one side. The most frequent queries include what causes lower back pain in females, lower right back pain, female lower back pain, right side back pain, and back pain in women. While pain may stem from gynecological or urinary systems, a large proportion of persistent cases are spine-related: discs, facet joints, sacroiliac (SI) joints, nerve roots, and muscle-fascia networks. As a specialty clinic, King’s Spine Centre evaluates spine-first causes while screening for non-spine contributors to ensure nothing serious is missed.
Women commonly report:
Lower right back pain female, sometimes radiating to the buttock or thigh
Lower back and pelvic pain female, which may feel deep or pressure-like
Dull pain in lower back female after sitting long hours or caregiving work
Lower back pain right side above buttocks that worsens when leaning back.

This guide explains what causes back pain in females, how to recognize patterns, what tests to consider, and which treatments help most. It is written for patient clarity and optimized to rank for high-value terms like what causes lower back pain in females, lower right back pain, female lower back pain, and back pain in women.
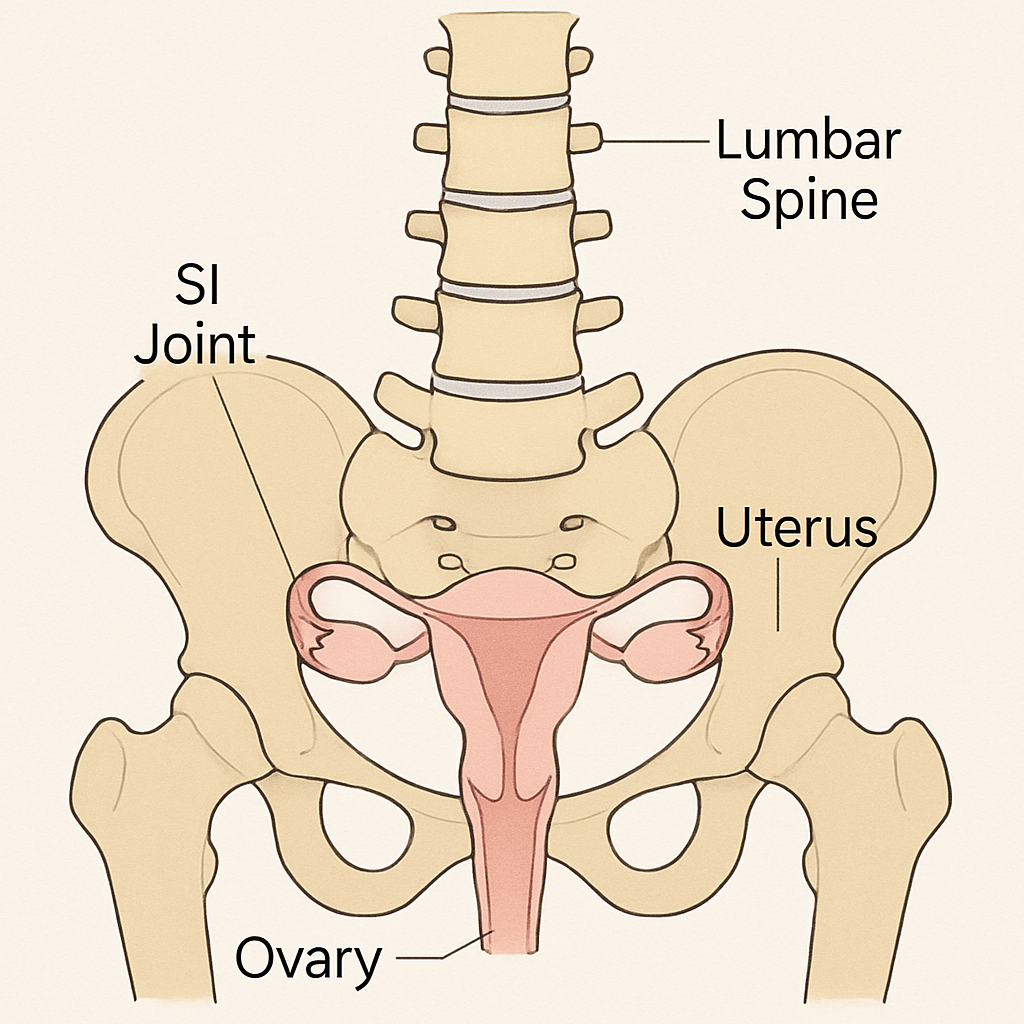
Female Spine Anatomy and Pain Generators
Understanding anatomy helps decode symptoms:
Intervertebral discs: shock absorbers that can bulge or herniate, triggering low back pain with or without leg symptoms (common reason for lower back and thigh pain female).
Facet joints: small stabilizing joints that can become arthritic or inflamed, often causing right side back pain or lower back pain right side that worsens with extension.
Nerve roots: can be compressed by disc material, bone spurs, or thickened ligaments, creating sciatica, numbness, or tingling.
Sacroiliac joint: a frequent driver of lower right side back pain female and buttock pain, especially postpartum.
Muscles and fascia: the multifidus, transversus abdominis, glutes, QL, and thoracolumbar fascia can all generate pain when weak, tight, or overworked.
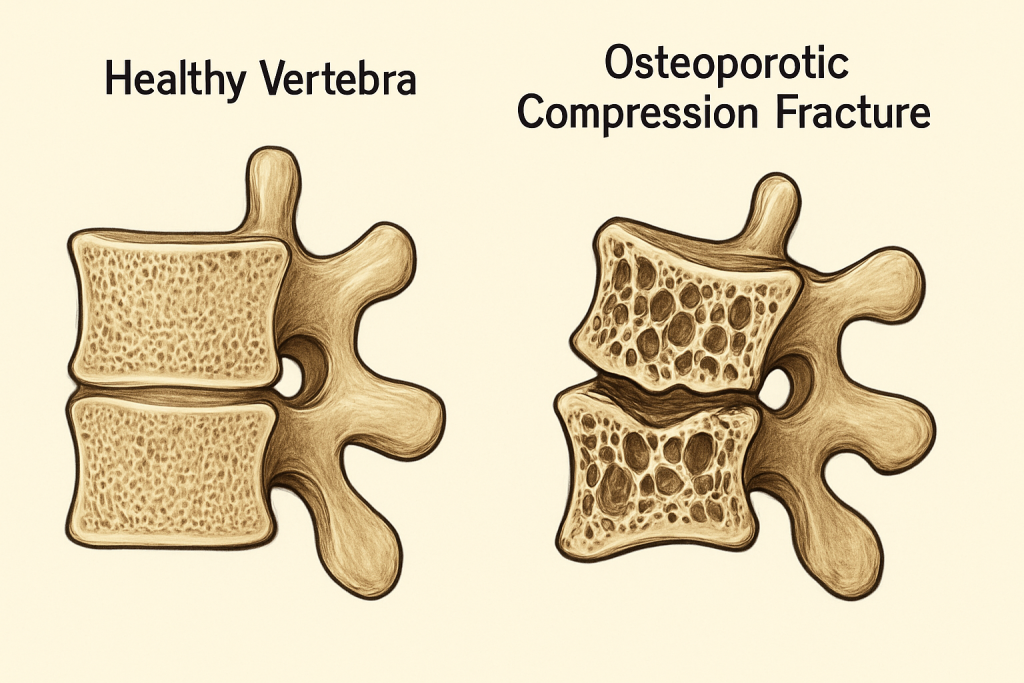
Vertebrae: weakened bones in menopause may develop compression fractures—sudden severe lower back pain female after minimal strain.
These structures explain why female lower back pain can be localized, on the right or left, or radiate to the hips, thighs, or pelvis. They also explain why lower back pain in women can overlap with pelvic discomfort.
What Causes Lower Back Pain in Females? Spine and Musculoskeletal Causes
This section focuses on spine-first causes most often seen at King’s Spine Centre.
Lumbar Disc Bulge and Herniation
What happens: The disc’s inner gel pushes against or through the outer ring, irritating nerves.
Symptoms:
Lower back pain with sitting and bending
Cough/sneeze or strain worsens pain
Leg pain, numbness, or tingling (radiculopathy)
Patterns: Right-sided herniations often create lower right back pain that can radiate to the buttock or down the leg. If pain tracks to the front pelvic area, it may reflect specific root involvement. High search terms apply here: what causes lower back pain in females, lower right back pain, female lower back pain, back pain in women.
Facet Joint Arthropathy
What happens: The facet joints become inflamed or arthritic.
Symptoms:
Focal right side back pain or left-sided pain
Worse with extension (leaning back), rotation, or standing
Tenderness over the paraspinal region
Associated phrase clusters include lower back pain right side above buttocks and right side lower back pain female.
Sacroiliac Joint Dysfunction
What happens: Inflammation or laxity in the SI joint connecting the sacrum and pelvis.
Symptoms:
Lower right side back pain female near the PSIS dimple
Pain with stairs, single-leg loading, turning in bed
Can refer to the groin or posterior thigh
Pregnancy and postpartum changes predispose this pattern.
Lumbar Spinal Stenosis
What happens: Narrowing of the canal or foramina compresses nerve roots.
Symptoms:
Back and leg pain with standing or walking; relief with sitting/bending forward
Heaviness, numbness, or tingling in legs
Often affects midlife and older women.
Spondylolisthesis (Vertebral Slippage)
What happens: One vertebra slips forward.
Symptoms:
Low back pain, worse with extension
Hamstring tightness; possible radicular features if foramina narrow
Osteoporotic Compression Fractures
What happens: Weakened vertebral bone collapses.
Symptoms:
Sudden severe lower back pain female after minimal strain
Increased pain standing or walking
This is a key scenario in postmenopausal women.
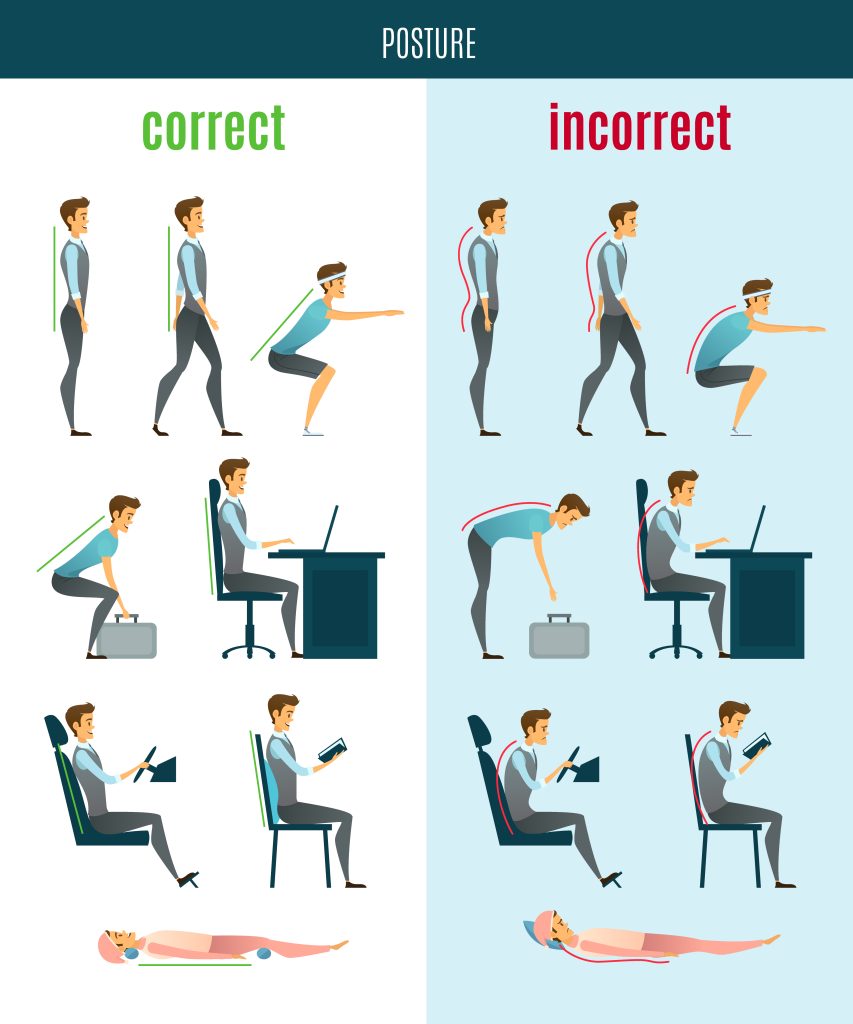
Myofascial Overload and Postural Strain
What happens: Weakness, tightness, and trigger points develop in lumbar and hip musculature.
Symptoms:
Dull pain in lower back female
Worse after long sitting or end of the day
This is common in desk-based roles and caregivers.
Menstrual and Hormonal Pain
Common: Lower back cramps female around periods, sometimes with pelvic heaviness.
Endometriosis Back Pain
Tissue similar to uterine lining grows outside the uterus.
Symptoms:
Lower back and pelvic pain female
May radiate to hips or abdomen
Multiple patients ask: can endometriosis cause back pain? Yes, endometriosis back pain is well-recognized.
Pregnancy and Postpartum Back Pain
Pregnancy adds load and relaxin-driven laxity; postpartum deconditioning can persist.
Common presentation: Lower back pain in women, lower right back pain female with SI joint involvement, and core weakness.
Ovarian/Uterine Causes of Lower Back Pain
Fibroids and cysts can create pelvic pressure and pain in lower abdomen and back female.
Urinary/Kidney Causes of Lower Back Pain
Kidney stones: sharp pain on the right side of back, pain in lower right back, sometimes radiating to abdomen/groin.
UTI/kidney infection: lower back pain and nausea female, fever, urinary frequency/urgency.
These should be distinguished from mechanical spine pain.
Right-Sided vs Left-Sided Pain: What Patterns Mean
Lower right back pain female that worsens with extension or twisting suggests right facet or SI joint stress.
Pain on the right side of back with sitting and bending points toward a right disc bulge.
Lower left back pain female also occurs with mirrored mechanisms—disc, facet, SI, or myofascial QL tightness.
Band-like waist discomfort may indicate myofascial strain or posture overload (reasons for lower back pain that are lifestyle-linked).
Red Flags: When Female Lower Back Pain Needs Urgent Care
Seek immediate attention for:
New severe back pain with trauma or in postmenopausal women (possible compression fracture)
Progressive weakness, numbness in saddle area, or bowel/bladder issues (possible cauda equina)
Lower back pain with fever, chills, nausea/vomiting, or urinary symptoms (possible kidney infection)
Lower back pain and vaginal bleeding or severe abdominal pain
Diagnosis at King’s Spine Centre: How We Pinpoint the Cause
History and Exam
Pain mapping: right lower back pain female vs bilateral symptoms
Mechanical vs inflammatory characteristics
Neurologic screen (strength, reflexes, sensation)
Special tests: straight-leg raise, slump, facet loading (extension-rotation), SI joint provocation (FABER, Gaenslen’s), hip screening, and core activation
Imaging
MRI: best for discs, nerves, stenosis, edema
X-ray: alignment, spondylolisthesis, fractures
CT: bony detail (pars defects)
DXA: bone density if osteoporosis suspected
Diagnostic Injections
Facet or medial branch blocks, SI joint injections: confirm pain generators; guide treatments like radiofrequency ablation
Treatments: From Conservative Care to Interventions and Surgery
Conservative First-Line
Analgesics and NSAIDs (as appropriate) for female lower back pain treatment
Heat for stiffness; ice for acute inflammatory flares
Physiotherapy to strengthen female lower back muscles and improve lumbopelvic control:
Multifidus and transversus abdominis activation
Glute medius/max strengthening
Neural mobilization for radicular pain
SI stabilization and hip mobility work
Manual therapy adjuncts
Short-term bracing in specific cases (e.g., post-acute, osteoporotic fractures)
Interventional Procedures
Epidural steroid injections for radicular pain from disc herniation/stenosis
Facet and medial branch blocks; radiofrequency ablation for longer relief of facet-mediated pain
SI joint injections for SI-driven lower back and pelvic pain female
Vertebroplasty/kyphoplasty for carefully selected osteoporotic fractures
Surgery (Minimally Invasive where suitable)
Microdiscectomy for persistent radicular pain with confirmed disc herniation
Laminectomy/laminotomy decompression for stenosis
Fusion for instability (e.g., high-grade spondylolisthesis) or proven segmental pain nonresponsive to comprehensive care
Postoperative rehab: core and hip strengthening, pelvic floor synergy, graded return to activities
Female-Specific Considerations: Hormones, Pregnancy, Menopause, and Bone Health
Hormonal phases can influence ligament laxity, affecting SI and facet joints
Pregnancy/postpartum: prioritize pelvic floor therapy, SI belts short-term, and progressive core rehab to address lower back pain in women
Menopause: bone density declines; screen for osteoporosis, support with resistance training and nutrition
Footwear and leg length discrepancy: correct asymmetries to reduce right side back pain or left-sided overload
Self-Care and Daily Roadmaps: Practical Relief for Back Pain in Women
Daily plan for female lower back pain treatment at home:
Morning mobility: 3–5 minutes of cat-camel, diaphragmatic breathing, gentle lumbar rocking
Microbreaks: stand and move 2–3 minutes every 30–45 minutes of sitting
10–12 minutes of core-lumbar conditioning:
Abdominal bracing with breath
Dead bug progression
Side plank (on knees initially)
Glute bridges
Bird dog holds
Hip mobility and posterior-chain care:
Hip flexor stretch, hamstring flossing, gentle QL release

Heat vs ice: ice for acute flares; heat for stiffness and myofascial tightness
Sleep positions: side-lying with pillow between knees or supine with pillow under knees to offload the lumbar spine
These steps help with lower right back pain, lower left back pain female, and general back pain in women.
Return to Work and Fitness: Graded Progression
Desk/office: ergonomic alignment, screen at eye level, lumbar support, task variability
Lifting: hinge at hips, neutral spine, exhale on effort, keep load close
Walking: start 10–15 minutes daily, increase 10–20% per week
Strength: two sessions weekly minimum focusing on glutes, hamstrings, quads, and core
Running: reintroduce once daily life is pain-managed; begin with walk-jog intervals
Pilates/yoga: valuable for control and mobility; avoid deep end-range flexion/rotation early in discogenic patterns
Myths vs Facts About Female Lower Back Pain
Myth: Bed rest cures back pain. Fact: Gentle movement and targeted exercise speed recovery.
Myth: All lower right back pain female is kidney-related. Fact: Many are mechanical—disc, facet, or SI joint.
Myth: Pain means stop all activity. Fact: Graded activity prevents deconditioning and chronicity.
Myth: Surgery is inevitable. Fact: Most cases improve with conservative care and, if needed, targeted interventions.
Why Choose King’s Spine Centre
Spine-first expertise for back pain in women, integrating gynecological and urinary screening when needed
Advanced diagnostics: MRI, targeted physical exam, and diagnostic injections to pinpoint lower back pain causes female
Comprehensive care: physiotherapy, interventional pain procedures, and minimally invasive surgery tailored to women’s needs
Women-focused rehab: core, glutes, and pelvic floor synergy for long-term resilience
Conclusion
Lower back pain in females is multifactorial and distinctly influenced by female biology, spinal anatomy, hormonal fluctuations, menstrual patterns, pregnancy, and menopause all shape risk and presentation. With 56–77% of women experiencing symptoms across the lifespan, including menstrual-related pain in up to 40–50%, pregnancy-related pain in about 70%, and vertebral fractures impacting roughly a quarter of postmenopausal women, the need for gender-specific evaluation and care is clear. Smaller average vertebral dimensions, greater spinal mobility, and hormonally mediated ligament laxity further underscore why back pain in women requires specialized assessment and treatment.
At King’s Spine Centre, care is tailored to these realities: integrating spine mechanics with reproductive health history, hormonal status, and female-specific risk factors to deliver precise diagnosis and targeted therapy. Early recognition and a comprehensive, women-focused plan can reduce pain, improve function, and prevent chronicity.
If lower back pain is disrupting work, sleep, or daily life, especially right side lower back pain female, persistent female lower back pain, or lower back pain right side above buttocks—book an evaluation at King’s Spine Centre. A personalized plan can speed recovery, prevent recurrences, and support a confident return to the activities that matter.
Frequently Asked Questions
Women experience higher rates of lower back pain due to anatomical differences including 10.6% smaller vertebrae, greater spinal curvature, hormonal fluctuations affecting ligament stability, and reproductive health factors like menstruation, pregnancy, and menopause.
Yes, 40-50% of women experience lower back pain during menstruation due to prostaglandin release, hormonal changes affecting ligament stability, and shared nerve pathways between the uterus and lower back muscles.
Pregnancy back pain affects 70% of pregnant women and is considered common due to weight gain, hormonal changes, center of gravity shifts, and increased spinal curvature. However, severe pain should be evaluated by healthcare providers.
Menopause increases lower back pain risk through decreased estrogen levels affecting bone density, accelerated bone loss, and changes in collagen synthesis affecting ligament integrity. 65% of perimenopausal women experience increased back pain.
Seek medical attention for severe pain with fever, cyclical pain with menstrual cycles, progressive weakness or numbness, loss of bowel/bladder control, or pain not improving with conservative treatment.
Yes, endometriosis causes lower back pain in 75.4% of affected women through compressed nerves, chronic inflammation, and increased prostaglandin production. The pain often correlates with menstrual cycles.
Female spines have 10.6% smaller vertebrae, greater lumbar lordosis, increased pelvic mobility, and different biomechanical loading patterns. These differences make women more susceptible to certain spine conditions and require gender-specific treatment approaches.
Scoliosis affects females 10 times more often than males before age 10, with faster progression rates and higher likelihood of requiring treatment. Women also demonstrate greater spinal mobility and different curve patterns compared to men.
Arthritis, osteoporotic fractures, inflammatory patterns, and sometimes visceral causes. Night pain with systemic symptoms warrants evaluation.
A combination of targeted physiotherapy for female lower back muscles, activity modification, ergonomic changes, and—in select cases—image-guided injections or minimally invasive surgery.
If severe, persistent beyond several weeks, associated with leg weakness/numbness, bladder/bowel changes, fever, or nausea—seek specialist evaluation.
Medical Disclaimer
This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your physician or a qualified healthcare provider regarding any medical questions or concerns.
Review Note
This content has been medically reviewed by the spine care team at King’s Spine Centre, Dubai, to ensure accuracy and relevance. Our team follows evidence-based guidelines and uses advanced diagnostic tools such as MRI and CT scans to evaluate spinal conditions.


